For a long time the placebo effect has been characterized as a false belief made-up in someone's head. But scientists know it's real. They have seen it in real-life observations of subjects and in the best double-blinded randomized clinical trials devised to test treatments for many diseases and conditions, especially those involving pain.
How and why the placebo effect occurs has remained a mystery; but recently, neuroscientists have discovered a key piece of the placebo effect puzzle.
Placebos are often used in what are called “sham” treatment groups. Individuals in these groups are given a pill or take part in an intervention designed to have no effect and used to contrast with the effects of the experimental condition.
However, given the brain's power — and perhaps its suggestibility — when individuals want to feel better, some experience improvement in their symptoms even from a treatment designed to do nothing. Sometimes these placebo effects are so strong that the people given sham treatments in clinical trials firmly believe that they are part of the group receiving the real active treatment being studied.It's not just members of the sham group who experience the placebo effect. Subjects in the “actual” treatment group also benefit from it.
It's not just members of the sham group who experience the placebo effect. Subjects in the “actual” treatment group also benefit from it. This is why it can be difficult for researchers to separate the benefits of a particular treatment from the placebo effect in clinical research testing therapeutic drugs and treatments.
The placebo effect has been seen in real-life observations and the best double-blinded randomized clinical trials devised for many diseases and conditions, especially pain. It muddies the results.
To understand what precisely is happening in the brain of someone experiencing the placebo effect, researchers at the University of North Carolina School of Medicine — with colleagues from Stanford, the Howard Hughes Medical Institute and the Allen Institute for Brain Science — set out to investigate brain pathways involved in pain.
Placebo analgesia is the term given when a person's positive expectation of pain relief is sufficient for patients to feel better. Brain imaging studies on humans showed increased neural activity in certain brain regions when the placebo effect was operating. Studies on mice also revealed that certain neurons and synapses are highly activated when mice expect pain relief and experience pain relief, even if no medication was involved.
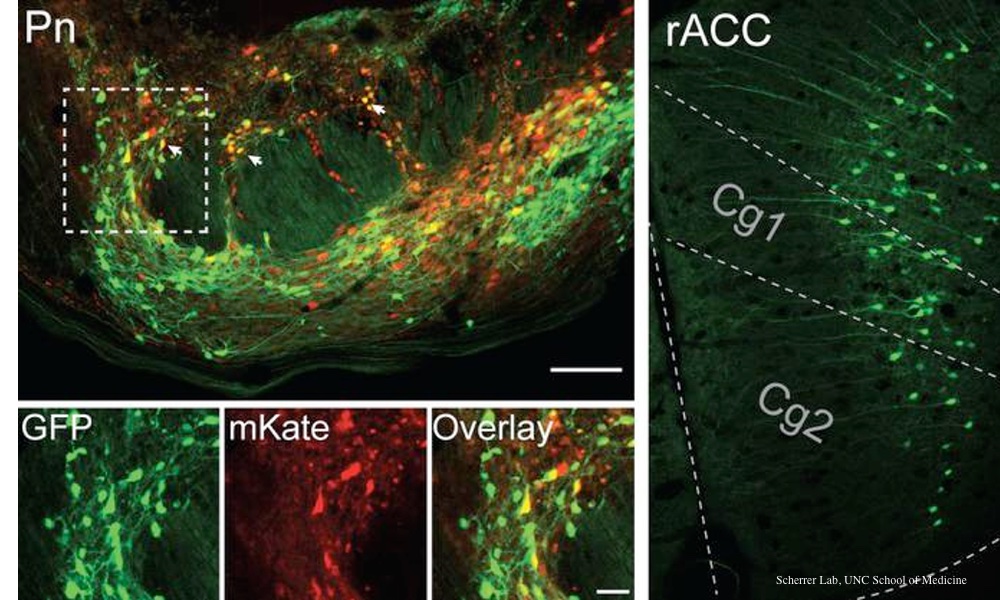
The images from those studies were not precise enough to show what was actually happening in those brain regions, so a team at the University of North Carolina designed a set of meticulous, complementary, and time-consuming, experiments to look — with single nerve cell precision — at activity in those regions.
What they found was a pain control pathway that links the cingulate cortex in the front of the brain, through the pons region of the brainstem, to the cerebellum in the back of the brain.
“That neurons in our cerebral cortex communicate with the pons and cerebellum to adjust pain thresholds based on our expectations is both completely unexpected, given our previous understanding of the pain circuitry, and incredibly exciting,” said Greg Scherrer, associate professor in the UNC Department of Cell Biology and Physiology.
“Our results do open the possibility of activating this pathway through other therapeutic means, such as drugs or neurostimulation methods to treat pain.”
After first developing a way to stimulate the expectation of pain relief in mice, the researchers then tracked what was happening in an area of the brain associated with the pain placebo effect: the anterior cingulate cortex (ACC).
The researchers used a variety of methods to study the intricate neurobiology of the placebo effect on brain circuits, individual neurons and synapses throughout the brain, including optogenetics — the use of light and fluorescent-tagged genes to manipulate cells.“We all know we need better ways to treat chronic pain, particularly treatments without harmful side effects and addictive properties.”
They found that when mice expected pain relief, that expectation boosted signals along a pathway of neurons in a brain area with no previously established function in pain or pain relief: the rostral anterior cingulate cortex projected its signals to nuclei in the pons.
“There is an extraordinary abundance of opioid receptors here, supporting a role in pain modulation,” Scherrer explained. “When we inhibited activity in this pathway, we realized we were disrupting placebo analgesia and decreasing pain thresholds. And then, in the absence of placebo conditioning, when we activated this pathway, we caused pain relief.”Sometimes these placebo effects are so strong that the people given sham treatments in clinical trials firmly believe that they are part of the group receiving the active treatment meant to help them.
The team also uncovered that certain cells in the cerebellum showed patterns of activity similar to those of the ACC neurons during pain relief expectation, suggesting evidence for the cerebellum's role in cognitive pain modulation, Scherrer and first author Chong Chen, a postdoctoral research associate in the Scherrer lab, said.
“We all know we need better ways to treat chronic pain, particularly treatments without harmful side effects and addictive properties,” Scherrer said. “We think our findings open the door to targeting this novel neural pain pathway to treat people in a different but potentially more effective way.”
The study is published in Nature.